top of page
Patient Presentation: A 23-year-old obese female was diagnosed with idiopathic intracranial hypertension (IIH) and referred to neurosurgery for ventriculoperitoneal shunt. A baseline ocular examination was performed prior to the procedure.
On examination, vision was 20/200 in the right eye, and 20/40 in the left eye. There was a right relative afferent pupillary defect. Slit lamp examination was normal.
A dilated fundus examination was performed demonstrating the following:
Uveitis
Case 20
Patient Presentation: A 30-year-old woman with no significant past medical history presented with subacute visual field loss in her left eye for 2 weeks. She described a paracentral scotoma OS with occasional flashes around the defect. She denied any history of autoimmune disease or recent upper respiratory tract symptoms. Visual acuity was 20/20 OU. Anterior segment exam was unremarkable.
Fundus photography and fundus autofluorescence were performed and are shown below:




OCT macula images were performed and are shown below:

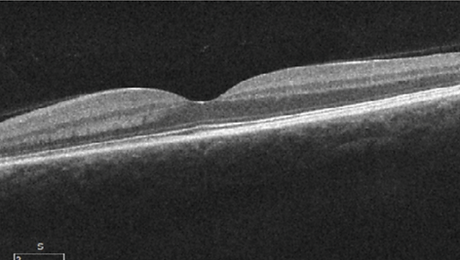
Question 1: What abnormality is seen on OCT macula in the left eye?
Question 2: How would you describe the abnormality seen in the fundus autofluorescence image of the left eye in this patient?
24-2 Humphrey Visual Fields were performed and are shown below:
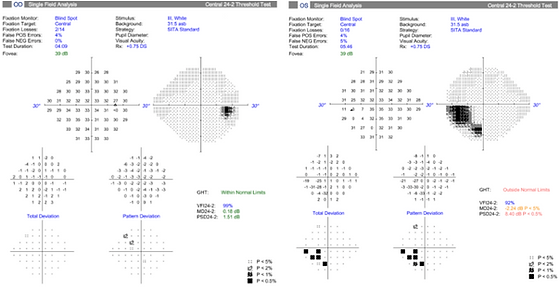
Question 3: Which of the following best describes the visual field defect seen in the left eye of this patient?
Question 4: Given the presentation of photopsias, an enlarged blind spot on visual field testing, and a trizonal pattern on fundus autofluorescence, what is the most likely diagnosis?
Question 5: Which of the following best describes the typical clinical course of AZOOR?
Question 6: What medication is most commonly used as the initial treatment for AZOOR in patients with progressive symptoms or outer retinal disruption on imaging?
Learning Objectives:
-
Recognize subtle outer retinal band loss seen in AZOOR.
-
Appreciate that AZOOR results in classic ‘trizonal defect’ appearance on fundus autofluorescence.
bottom of page
.png)