top of page
Patient Presentation: A 23-year-old obese female was diagnosed with idiopathic intracranial hypertension (IIH) and referred to neurosurgery for ventriculoperitoneal shunt. A baseline ocular examination was performed prior to the procedure.
On examination, vision was 20/200 in the right eye, and 20/40 in the left eye. There was a right relative afferent pupillary defect. Slit lamp examination was normal.
A dilated fundus examination was performed demonstrating the following:
Retina
Case 86
Patient presentation: A 40-year-old male presented to a tertiary retina service with a 4-day history of sudden-onset large central scotoma in the left eye. He had no prior ocular or family history of eye disease, no history of coagulopathies, and no head or neck trauma. His past medical history was otherwise unremarkable. He was taking semaglutide (Ozempic) for weight loss and was recovering from an upper respiratory tract infection.
On examination, his visual acuity was 20/20 in the right eye and CF in the left eye. IOP was 13 mmHg OU. There was no RAPD. Anterior segment examination was normal in both eyes. Posterior segment examination of the right eye was normal. Posterior segment examination of the left eye revealed a large pre-macular hemorrhage. OCT macula of the left eye is shown below:
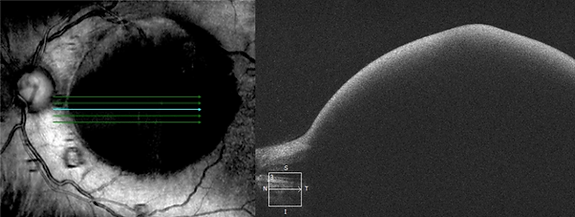
Question 1: Describe the OCT.
Question 2: What is the diagnosis?
Question 3: What is the initial treatment for this patient?
References:
-
Duane TD. Valsalva hemorrhagic retinopathy. Trans Am Ophthalmol Soc. 1972;70:298-313.
-
Mathew DJ, Sarma SK. Valsalva retinopathy with double ring sign: Laser membranotomy for twin bleeds. Saudi J Ophthalmol. 2016;30(1):68-70. doi:10.1016/j.sjopt.2015.10.003
-
Durukan AH, Kerimoglu H, Erdurman C, Demirel A, Karagul S. Long-term results of Nd:YAG laser treatment for premacular subhyaloid haemorrhage owing to Valsalva retinopathy. Eye (Lond). 2008;22(2):214-218. doi:10.1038/sj.eye.6702574
Learning Objectives:
-
Recognize the clinical and OCT features of Valsalva retinopathy.
-
Understand the management and treatment of Valsalva retinopathy.
bottom of page
.png)