top of page
Patient Presentation: A 23-year-old obese female was diagnosed with idiopathic intracranial hypertension (IIH) and referred to neurosurgery for ventriculoperitoneal shunt. A baseline ocular examination was performed prior to the procedure.
On examination, vision was 20/200 in the right eye, and 20/40 in the left eye. There was a right relative afferent pupillary defect. Slit lamp examination was normal.
A dilated fundus examination was performed demonstrating the following:
Neuro-Ophthalmology
Case 8
Patient Presentation: A 31-year-old male is referred to the ophthalmology clinic. He suddenly developed an inferior visual field defect in the left eye 9 months ago that persisted. He was unable to seek medical care at the time. On exam, BCVA is 20/20 OU and Humphrey visual field testing showed a left inferior central scotoma and is shown below.


Question: What is the differential diagnosis of this visual field defect?

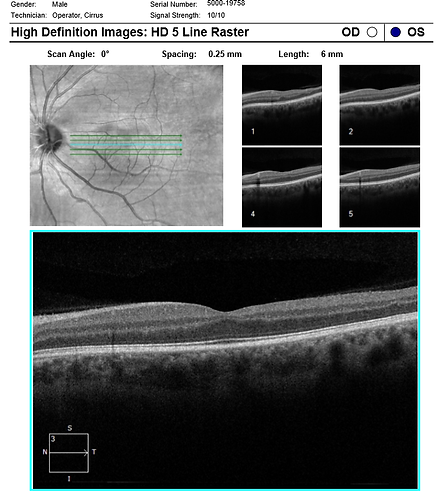
Question: A fundus photo and OCT macula OS are shown above. What OCT protocol would be helpful in differentiating the cause?

Question: OCT macula OS with vertically oriented line scans is performed and shown above. The retina highlighted in yellow is ________ in relation to the fovea.

Question: What is the main abnormality seen on the OCT?
Question: Based on the OCT findings, clinical presentation, and fundus description, what is the diagnosis for this patient?
References:
1. Hayreh SS, Podhajsky PA, Zimmerman MB. Branch retinal artery occlusion: natural history of visual outcome. Ophthalmology. 2009;116(6):1188-94.e944.
2. Ghazi NG, Tilton EP, Patel B, Knape RM, Newman SA. Comparison of macular optical coherence tomography findings between postacute retinal artery occlusion and nonacute optic neuropathy. Retina. 2010;30(4):578-85
Learning Objectives:
1. To diagnose and classify chronic BRAO using OCT findings
2. To understand the management plan for patients with chronic BRAO
bottom of page
.png)